What is lumbar spinal stenosis?
Anatomy of the spine
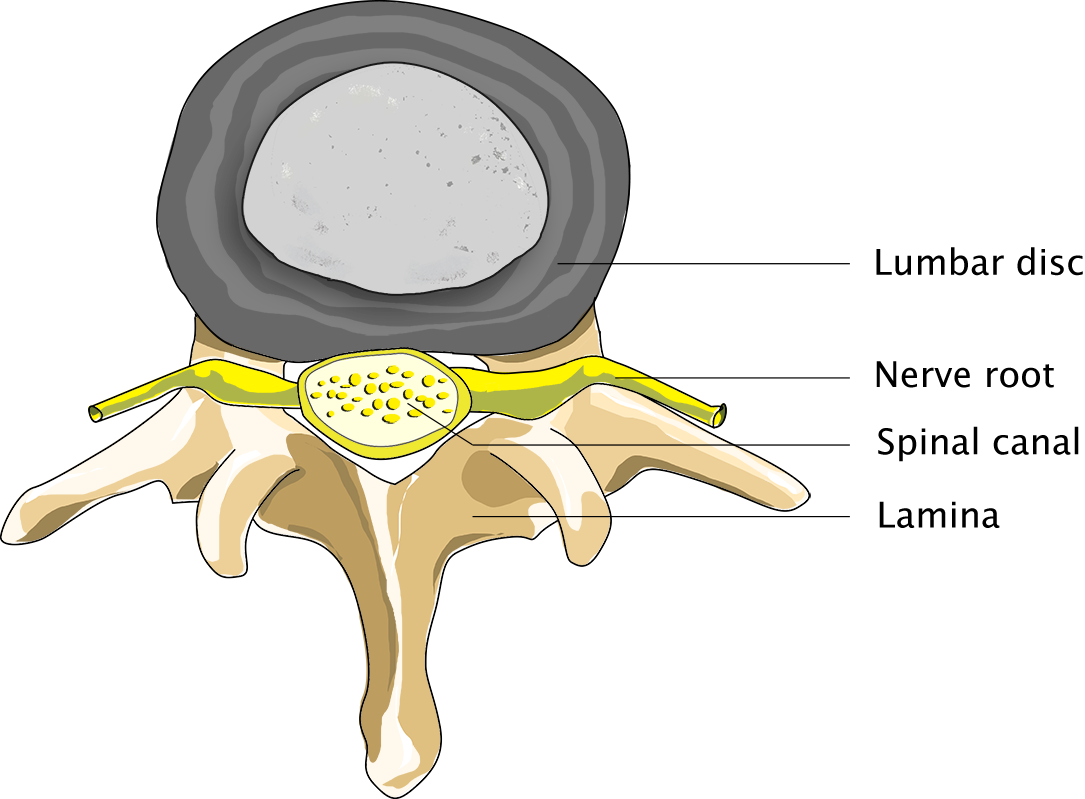
The spinal column is located at the heart of the musculoskeletal system. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, 5 lumbar vertebrae and the sacrum. Intervertebral discs are located in between the vertebrae, and these 23 discs increase the spine’s elasticity and mobility. They also serve as shock absorbers.
The spinal canal
The spinal canal is positioned at the centre of the spine. Vertebral arches (with spinous processes) are located at the back of the canal. Although spinal stenosis can occur at any level of the spinal canal, it most commonly occurs in the neck and the lower back.
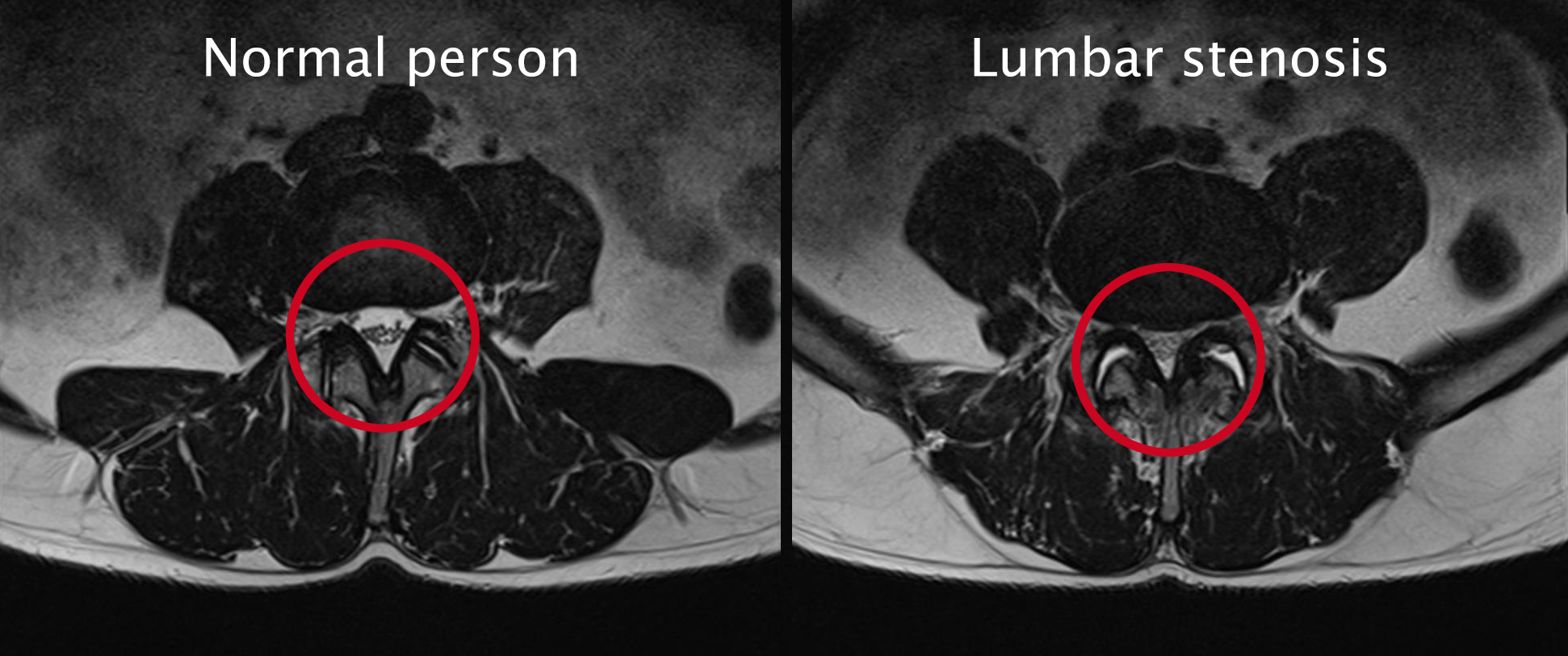
Normal person
Person suffering from lumbar spinal stenosis
In this article
Use the overview below to read more about a specific topic:
Causes of a lumbar spinal stenosis
Degeneration of the spine
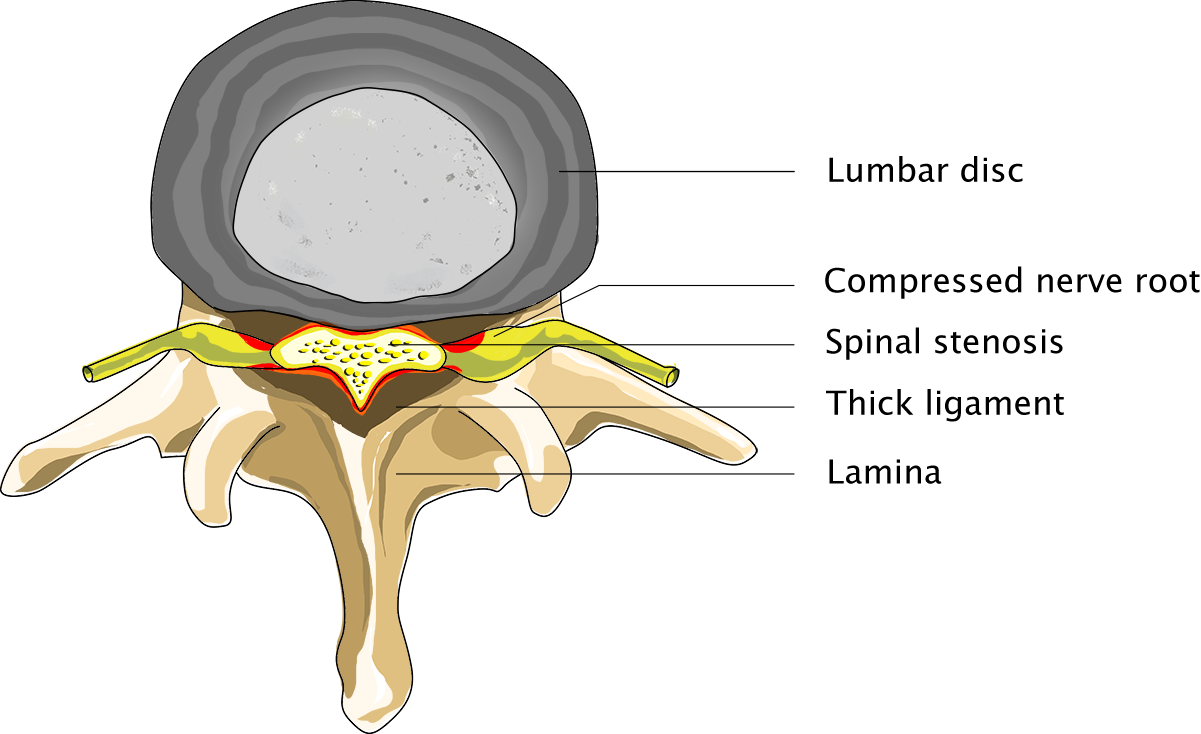
Degeneration of the spinal column is a normal process to which everyone is prone to some degree. Some people naturally have narrower spinal canals than others.
When the spine begins to degenerate, the bands (ligaments) between the vertebrae thicken. In addition, the small facet joints, which overlap and connect the vertebral arches on the back of the spine, enlarge (which is to say they become wider and flatter). As a result, the nerve roots will have less space, especially in the small groove where the nerve roots leave the spinal canal. In some cases, a bulging intervertebral disc may contribute to the narrowing of the spinal canal.
Symptoms of a lumbar spinal stenosis
Pain in both legs
Only nerves pass through the bottom of the spinal canal. Pain and other symptoms are caused by the pressure being exerted on these nerves. As a result, symptoms may resemble those of a hernia. Many patients will suffer from pain in both legs, which will become more intense when they are walking. As a result, the symptoms rather resemble those of peripheral vascular disease.
Patients will experience pain when walking. Sometimes they will also experience numbness and/or a loss of strength in their legs. The pain will quickly subside when such patients take a break from walking, especially when they bend over, crouch or sit down. This is because walking will cause the spine to bend a little more, which will increase the amount of pressure exerted on the nerve. The narrowing of the spinal canal will subside a little when the patient bends over or crouches. Therefore, patients suffering from lumbar spinal stenosis are generally quite able to ride a bike. They generally prefer to lean on a trolley when out grocery shopping.
Diagnosis of a lumbar spinal stenosis
Physical examination
In addition to listening to the patient’s complaints and performing a thorough neurological examination, the neurosurgeon will carry out a medical imaging procedure. MRI of the lumbar spine is the first examination of choice and generally shows the abnormality in great detail. Additionally, a CT scan may be performed to obtain a better understanding of the patient’s bone structures.

Diagnosis of a lumbar spinal stenosis
Diagnosis of a lumbar spinal stenosis
Finally, the surgeon will have to rule out the possibility that the patient’s discomfort and other symptoms are caused by a vascular disorder in the patient’s leg, since such a disorder presents with the same symptoms. This is easy to determine in a physical examination, by palpating the legs and feet. If it is hard to feel a pulse in the legs and feet, an additional peripheral vascular examination will have to be performed first.
Surgery of a lumbar spinal stenosis
Surgical treatment
Generally speaking, it is quite obvious from a patient’s symptoms and experiences and from the examination results whether a patient requires surgery or not. Even so, it is up to the patient to decide whether or not s/he wishes to undergo surgery, because only the patient knows the severity of the discomfort s/he is experiencing.
In order to remove the stenosis, the patient is operated on from the back of the spine. This procedure is called bony decompression and involves making a small incision in the middle of the lower back, exactly above the level of the stenosis. The spinal canal is opened between the back muscles and two vertebral arches, and excess connective tissue and bone tissue are removed, to the extent necessary, so as to relieve the compressed sciatic nerves branching off the spinal canal.
So what happens when I undergo surgery?
Click the button below for some general information on operations performed by Dr Schröder.
Risks of lumbar spinal stenosis surgery
Potential post-operative complications
Like any other operation, lumbar spinal stenosis surgery carries a few risks. However, complications are highly unlikely to occur. After all, lumbar spinal stenosis operations are carried out many times a year at our clinics.
Even so, we may encounter some neurological failure after the operation. This is generally caused by the fact that the nerve, which had been compressed for a long time, had to be manipulated during the operation. Common risks also include inflammation or a wound that will not heal properly. Subsequent bleeding is a very rare but highly unpleasant complication. The well-known cerebrospinal fluid leak is another, none too severe complication. A fluid leak is a tiny tear in the sac that holds the cerebrospinal fluid. When this happens during surgery, the leak will be sealed at once, and it will not have any lasting consequences. In very rare cases the tear will continue to leak. If this happens, the tear will have to be resealed at a later stage.
After surgery of a lumbar spinal stenosis
Tips from a physiotherapist
Following the operation, the patient’s follow-up appointments will be with a physiotherapist, who will provide some useful tips to help the patient load his back and make a full recovery while the patient is still at our clinics. Typically, patients are able to walk again the day after their operation. They are free to go home, then, depending on the size of their wound.
Follow-up examination
Two weeks after the operation, the patient will be called for a phone check-up during which his or her current condition will be discussed. Generally, the patient will be told on this occasion that s/he is allowed to resume normal activities and increase the load on the back. If the patient is already experiencing a clear improvement, no further steps will have to be taken at this point.
Resuming exercise and returning to work
The patient will be allowed to undergo supervised physiotherapy upon his or her discharge from the clinic if s/he is in a poor physical condition or afraid to start moving again. Embarking on an intensive back and abdominal muscle training programme soon after the operation is not recommended, as the back muscle will not have full pulling force for the first 3 to 6 months following surgery. The duration of the post-operative recovery period differs from patient to patient. Whether or not a patient will be allowed to return to work soon after an operation obviously depends on the nature of the person’s duties. Patients should always listen to their bodies and take a break whenever their bodies tell them they have had enough.






