What is spinal instability?
Increased mobility between one vertebra and another
Back and leg aches may also be caused by spinal instability, which may be caused by degeneration of the intervertebral disc, degeneration of the facet joints between the vertebrae and thickening of the bands of connective tissue between the vertebral arches. This causes a narrowing of the spinal canal and increased mobility between one vertebra and its neighbour, which in turn may cause a vertebra to be displaced. Depending on the severity of their symptoms, patients may or may not benefit from surgery.
Patient suffering from spinal instability
Hernia operations are among the procedures most frequently carried out by neurosurgeons. Out of nearly 11,000 hernia operations performed in the Netherlands each year, over 9,000 are carried out by neurosurgeons.
In this article
Use the overview below to read more about a specific topic:
Causes of spinal instability
Displaced vertebra
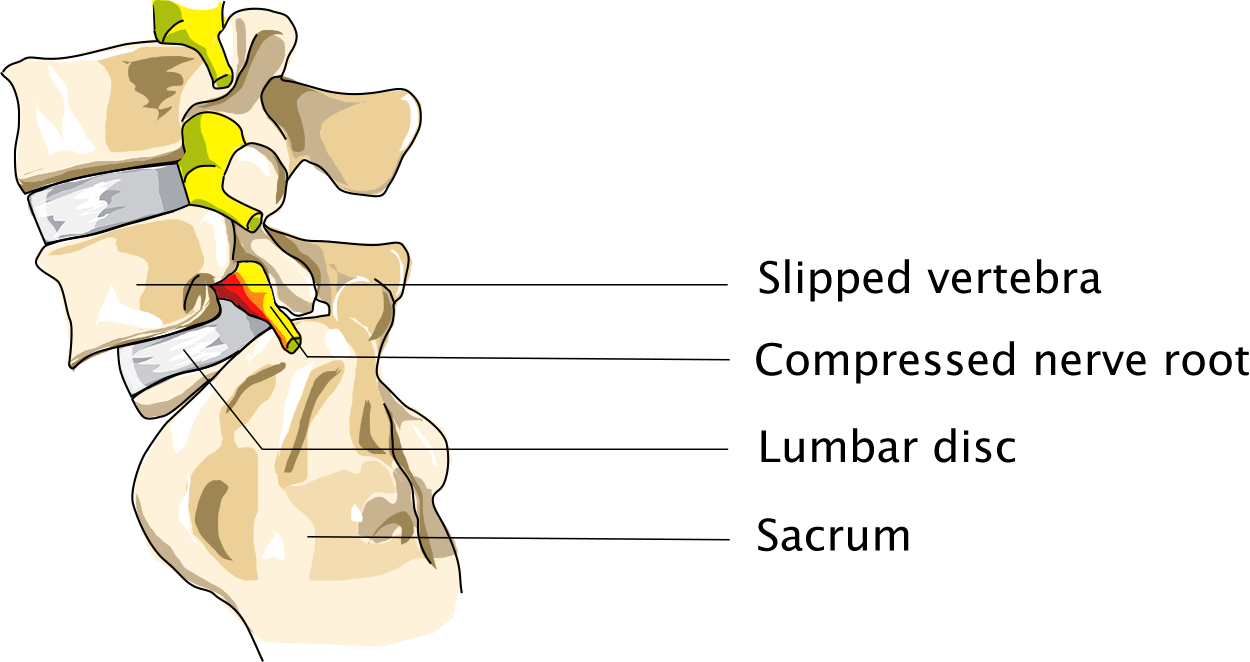
So-called spinal instability due to a displaced vertebra is an automatic indication for surgery. Such instability may be caused on the one hand by a congenital reduction defect of a vertebral arch, which is preventing the facet joints of a vertebra from being properly aligned. This generally happens in the lower part of the spine, and may result in the displacement of a vertebra at a relatively young age.
Symptoms caused by ageing
In addition, spinal instability may be caused by degeneration due to ageing. In a way, these are symptoms of old age, which some people will experience at a younger age than others. Symptoms include increasing inelasticity of the intervertebral disc, enlarged joints between the vertebral arches (facet joints) and thickening of the bands (ligaments) between the vertebral arches. All these things cause narrowing of the spinal canal, as well as increased mobility between the vertebrae. As a result, vertebrae may be displaced vis-à-vis each other.
Degenerative Disc Disease (DDD)
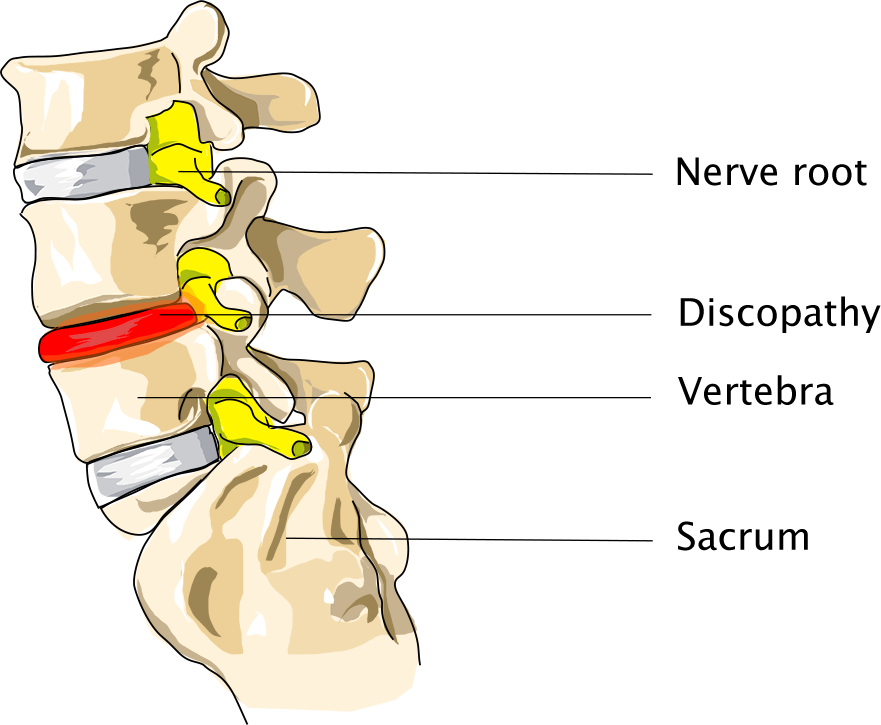
What the discussion is really about, is the question as to whether such increased mobility without any vertebrae actually having been displaced must be considered spinal instability, and whether this is causing the symptoms. This situation is known among doctors as degenerative disc disease. Opinion is divided on the subject, but research is increasingly proving that degenerative disc disease is a separate disorder (1).
Scientists are increasingly convinced that backache may be caused by degeneration of the intervertebral disc, which may lead to ‘micro movements’ even though X-ray images show no clear signs of displacement. This minimally increased mobility results in both pain and ongoing degeneration, thus creating a vicious circle.

Black Disc
*1. Ann Rheum Dis. 2013 Jul; Novel genetic variants associated with lumbar disc degeneration in northern Europeans: a meta-analysis of 4600 subjects.
Failed Back Syndrome
Even after several hernia operations all tackling the same spot (in the event that the hernia relapses), the quality of the intervertebral disc will decrease, as will its ability to absorb shock. As a result, while a patient’s leg may be less sore after each follow-up operation, the quality and functioning of the intervertebral disc will increasingly deteriorate, and the patient will increasingly suffer deep backache.
Symptoms of spinal instability
Displaced vertebra
If the degenerative process causes spinal instability, displacement of one vertebra will cause the spinal canal to narrow, thus causing the constriction of one or more sciatic nerves, which may cause pain radiating down the legs as well as low backache. If this happens, both legs will often be affected
Generally speaking, when a vertebra is displaced, the patient is already experiencing narrowing of the spinal canal due to thickened ligaments and enlarged vertebral facet joints, which are common in this situation. This will cause additional narrowing of the spinal canal, which in turn will cause more pain. Patients suffering from a displaced vertebra tend to experience more pain in their legs than in their lower back.
Degenerative disc disease
Scientists are increasingly convinced that backache could be traced back to degeneration of the intervertebral disc, which causes the spine to become unstable. It is believed that affected vertebrae make ‘micro movements’, even though no clear displacement can be detected in X-ray images. This minimally increased mobility results in pain on the hand and in ongoing degeneration on the other, thus causing a vicious circle. Patients suffering from degenerative disc disease tend to suffer deep backache rather than sore legs.
Patients will often experience pain in their legs, as well, but they will suffer a less specific type of pain than the one caused by mechanical nerve compression, which may occur in the event of a hernia or displaced vertebra. This is called pseudoradicular leg pain. It is said that the pain in the legs is caused by an inflammation of the degenerated intervertebral disc, which causes endotoxins and radicals to be released that will irritate the adjacent sciatic nerve/s.
The deep backache will be most painful during the day, when the back is being loaded and used, and will generally subside during the night.
Diagnosis of spinal instability
How is spinal instability diagnosed?
Displaced vertebra
The patient will first be examined by a neurologist. Depending on what s/he is told by the patient, the neurologist may also perform a medical imaging procedure, which will often enable him or her to make a diagnosis.

Diagnosis of spinal instability
Degenerative Disc Disease
Medical imaging procedure
Here, too, the patient will first see a neurologist, after which they will often undergo one or more medical imaging procedures – generally, an X-ray photo and an MRI scan. A radiologist will then often describe one or more intervertebral discs that show up black in the images and must therefore be dehydrated (so-called ‘black discs’).
Degenerative disc disease (DDD)
Sometimes an image will show a ‘modic sign’, i.e., an inflammation of the degenerated intervertebral disc in the adjacent vertebrae. Quite often the height of the intervertebral disc will have decreased, thus reducing the disc’s ability to do what it is supposed to do, i.e., absorb shock and keep the adjacent vertebrae mobile.
Plaster corset
If the patient’s symptoms are reduced when s/he is not using his or her back much, a plaster corset may be used to predict the results of an operation whereby a part of the spine is temporarily immobilised from the outside. Such a test corset covers the upper legs and is generally worn for two weeks. While wearing the corset, the patient will be able to walk, lie down and go to the toilet as usual. However, s/he will be unable to bend over and sit down.
Discogram
A discogram may help the doctor make a correct diagnosis. If the patient’s doctor suspects an intervertebral disc is the source of the patient’s pain, he may request that some contrast agent be injected into the disc to determine whether or not the pain becomes more intense. He will subsequently request that a numbing agent be injected into the disc. If the pain then subsides, this may be a sign that the intervertebral disc is involved in the patient’s problems.
This test will be performed by an anaesthetist at our clinics. You will see him or her for an intake interview before being subjected to the test in a separate appointment. The test will take half a day of your time, and you will have to be dropped off and picked up from the clinic by someone else. Since this test involves a temporary anaesthetic, if your deep backache returns, you will first have a telephone appointment with the anaesthetist to discuss the results of the test.
Psychological evaluation
The standard protocol may include a psychological evaluation, which is designed to provide our doctors with an insight into how the patient is dealing with his or her symptoms, what he or she expects from an operation, and what type of rehabilitation procedure might suit him or her best. None of these predictive evaluations will be 100% accurate. Once all tests have been completed, the patient may schedule a follow-up appointment with the neurosurgeon to discuss the results. Depending on the test results, the surgeon may propose that the patient undergo surgery
Surgery of spinal instability
In consultation with the patient, the neurologist will always seek to treat the patient’s symptoms in a non-surgical manner for as long as possible. If, in the course of time, it turns out that regular therapy is no longer effective, the neurologist will refer you to a neurosurgeon to discuss surgery. Surgery must always be considered a final treatment option.
Spondylodesis
Spondylodesis is a technique designed to join vertebrae. The following section specifically discusses joining the vertebrae of the lumbar spine. This is the lowest part of the spine, which is most prone to degeneration. Spondylodesis is a technique which has been employed for years, but which has become much more popular lately due to the recent availability of modern materials and technologies which make the procedure safer and more effective. On the down side, some doctors may be a little too keen to prescribe this operation. The decision to undergo this type of surgery should not be made lightly; it should be well informed and well considered.

Robot used to fuse vertebrae
There are several approaches to joining vertebrae, and several technologies that can be employed. For instance, the vertebrae can be accessed from nearly all sides: from the back, from the side and from the front. Each approach has its pros and cons. The surgeon will decide on an approach on the basis of the patient’s symptoms and the cause of these symptoms.
From the back (PLIF/TLIF))
At our clinics, spondylodesis is performed in a minimally invasive manner, which is to say through tiny incisions, thus causing the back muscle to remain largely in place. First one or more compressed sciatic nerves will be released through a four-centimetre incision in the middle of the back (PLIF) or a little to the side of the back (TLIF), by removing excess bone tissue, connective tissue and the protrusion of the intervertebral disc. Then the remainder of the intervertebral disc will be removed, to the extent that such is possible. Next the vertebrae will be joined. A little cage will then be placed in the disc space, after which the disc space will be filled with chips of the patient’s own bone, obtained from the excess bone tissue removed during the first part of the operation. This will help the vertebrae fuse properly. The direction of the screws that are to be implanted will be determined by a mini-robot called a Renaissance robot, using a thin metal rod. This will help the surgeon place the screws even more precisely, which will minimise the risk of additional nerve damage. Once the steel rods have been installed, hollow screws can be placed over these rods and screwed into the vertebrae, after which the connecting rods will keep the two screws on each side together.
In order to implant the screws and rods, we will use the Sextant system, which will enable us to insert both the screws and the rods through small incisions in the patient’s skin. This tends to be more effective than open surgery in terms of the amount of damage sustained by the muscles. The system is named after a navigation tool once used by seafarers, which it somewhat resembles.
From the front (ALIF)
Patients who suffer degenerative disc disease are generally operated on from the front. After all, the sciatic nerves that leave from the spinal canal at the back of the spine are not being mechanically compressed, so there is no reason to join the vertebrae from the back.
The ALIF procedure is performed by gaining access to the patient’s abdominal cavity. The procedure involves removing an intervertebral disc from the front of the spine, after which a small fusion cage filled with cement will be placed in the now-empty space and fixed with four additional pedicle screws, so that there will be no more mobility between the vertebrae. In this way the vertebrae will be kept apart, and they will slowly fuse.
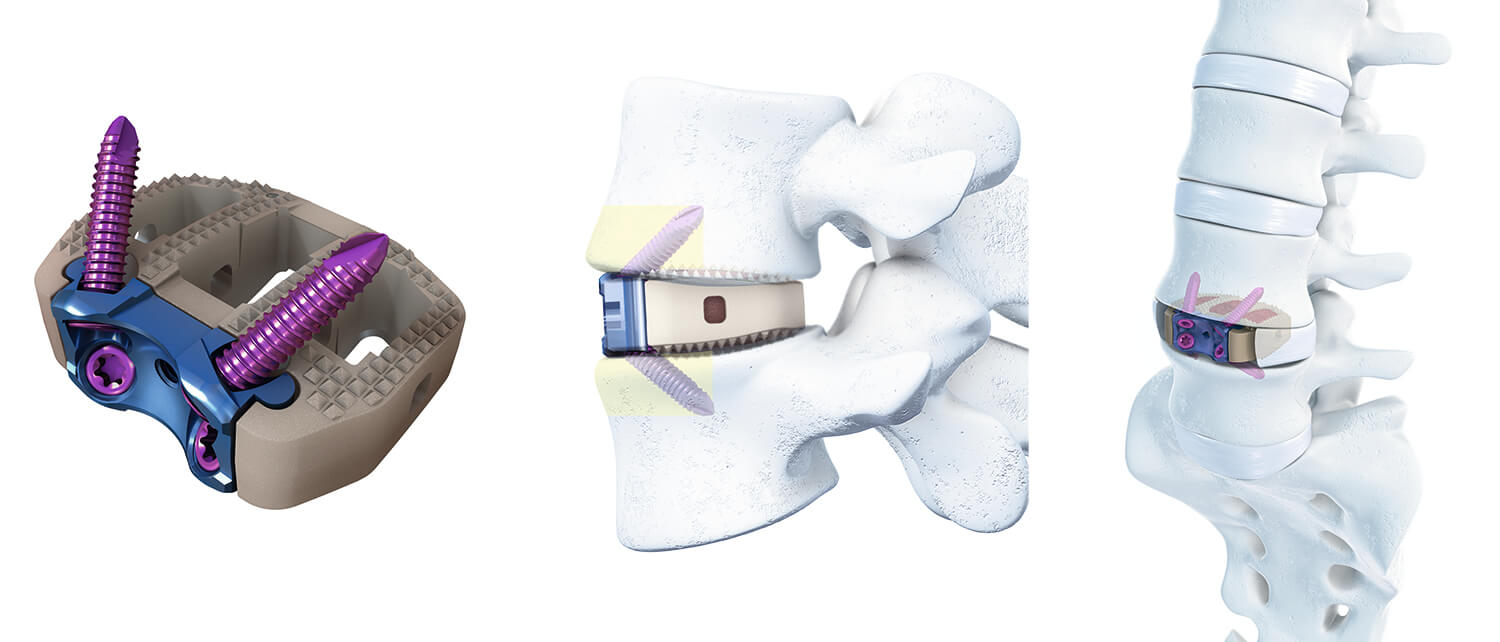
Synfix (DePuy Synthes)
Minimally invasive techniques
There are many different minimally invasive techniques and methods, and there is no best method. The choice as to which method to use depends on the surgeon’s preferences and the patient’s situation. However, I do take the following things into account:
- 'If I can achieve the same result with a small incision, why would I make a large incision?'
- '2. I’ll make my incision as small as possible, and as large as necessary'.
So what happens when I undergo surgery?
Click the button below for some general information on operations performed by Dr Schröder.
Risks of spinal instability surgery
Operation from the back (PLIF/TLIF)
To a large extent, the risks associated with PLIF procedures are identical to those associated with any spinal surgery. However, in addition to these risks, there are risks associated with inserting the materials and with the materials themselves. The procedure requires a significant amount of nerve manipulation, which may cause nerves to stop functioning properly or stop functioning altogether. The inserted materials may come loose, break or shift. Even very experienced surgeons who use the right techniques cannot entirely prevent such complications from occurring. Fortunately, such complications are quite rare.
Operation from the front (ALIF)
In addition to the aforementioned risks, there is a very slim chance of gastrointestinal perforation, since the incision is made close to the intestines.
Careful selection of patients
Since various types of materials are now available for implantation, spondylodesis has become very popular recently. Unfortunately, not all doctors seem to understand when there is an indication for this type of surgery. The more carefully the patients are selected, the better the results. For some patients, spondylodesis is a ‘last resort’. Such patients will have tried everything else, are desperate to be healed and therefore may have overly high expectations of the procedure. It is vital that patients make a well-informed and well-considered decision.
After surgery of spinal instability
Operation results
When assessing the results of an operation, a surgeon and his or her patients may have different points of view. In other words, it is entirely possible that a surgeon has obtained a technically excellent result, even though his or her patient is not the slightest bit happy. Scientists tend to judge operations by the degree to which a complete bony fusion has been brought about. However, it has proven to be extremely difficult to determine the extent to which this has happened, and moreover, success in this respect does not always match the patient’s satisfaction rate (the clinical result).
If the vertebrae are joined purely to reduce backache, the success rate is likely to be 40 to 50%. If patients only suffer abnormalities at one single level and do not suffer any other problems, the success rate may be as high as 80 to 85%, provided that the patients have been carefully selected. These numbers have been like this for years, despite many attempts to select only patients who are sure to benefit from the operation.
Clearly, it remains very difficult to predict how certain patients will respond to this type of surgery, which means that about half of patients undergoing spondylodesis will go under the knife in vain, despite their high expectations. Unfortunately, this may give spondylodesis a bad reputation.
Less impressive results in smokers
Smokers are much less likely to benefit from spondylodesis than non-smokers. They are also less likely to achieve a stable bony fusion. Therefore, surgeons in the United States tend not to perform spondylodesis on patients who smoke. Our clincs, too, will not perform this type of surgery until it has been established that the patient is not a smoker or has quitted smoking.






