What is spinal hernia?
A bulge in the intervertebral disc
Spinal disc herniation is a bulge in an intervertebral disc. This bulge presses on a sciatic nerve, thus causing pain in a patient’s leg, which may or may not be accompanied by symptoms of neuropathy (numbness or loss of strength).
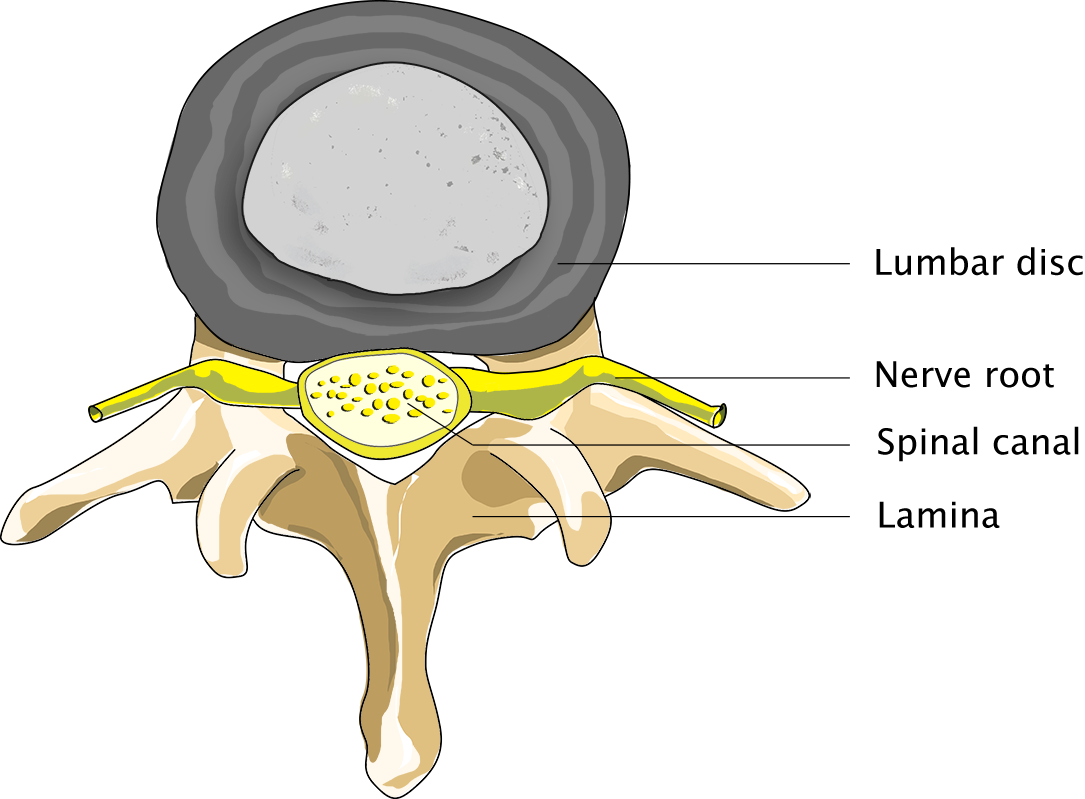
Normal person
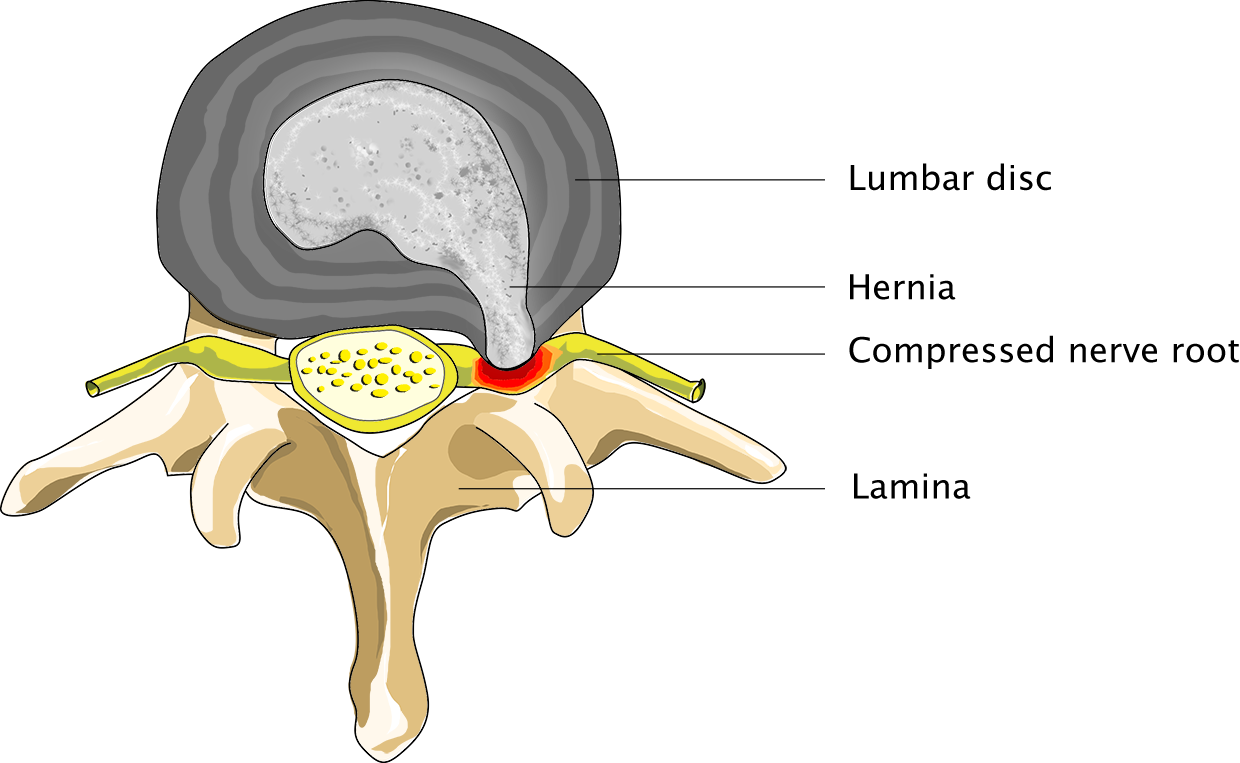
Patient suffering from spinal hernia
Hernia operations are among the procedures most frequently carried out by neurosurgeons. Out of nearly 11,000 hernia operations performed in the Netherlands each year, over 9,000 are carried out by neurosurgeons.
In this article
Use the overview below to read more about a specific topic:
The cause of backache is unclear
What happens even more often is that neurosurgeons will see patients suffering from backache. In many cases, it will be unclear at first whether a patient’s backache is caused by a hernia. Doctors used to assume that this was the case. However, these days, it is generally believed that degeneration of an intervertebral disc may contribute to the onset of backache.
Some hernias do not present with pain symptoms. A hernia typically presents with pain radiating down one leg, since the hernia causing the pain is generally to one side of the spine. However, hernias do occur in the middle of the spine, which may cause pain radiating down both legs.
Causes of a spinal hernia
Degeneration of an intervertebral disc
Degeneration of an intervertebral disc is a normal process that occurs in all of us to some extent. Heavy work involving frequent bending over and lifting of heavy objects may put a person at an increased risk of developing backache, but will not cause a hernia. Hernias occur in equal measure in people performing manual labour and in people who have office jobs. What is notable is that smokers require spinal hernia surgery much more often than non-smokers, and that surgeries performed on smokers tend to be less successful than those performed on non-smokers. Persons with jobs involving a lot of sitting, e.g. drivers and office workers, are especially prone to hernias.
A hernia can affect anyone
If an intervertebral disc degenerates, it may start bulging, or alternatively, its outer ring may tear, thus causing pieces of the soft core to be pressed through this tear, towards the spinal canal. Generally speaking, the ring will tear in its weakest spot, which happens to be the spot where the sciatic nerve branches off the spinal canal. A hernia can affect anyone, and we do not know why some people are affected while others are not. However, it is known that some families are more prone to hernias than others.
Symptoms of a spinal hernia
Generally preceded by backache
Generally speaking, the onset of a hernia is preceded by backache. The great majority of patients will have experienced lumbago. However, a spinal hernia does not just affect the back, but radiates down a leg and may present with numbness or pins and needles. The pain affects the area served by the sciatic nerve, on which the hernia is pressing. Pressure on this nerve may also result in a loss of strength in a leg or foot muscle.
Paralysis or a tingle
Nerves serve a dual function: they serve the muscles, but also an area of skin. Each nerve serves its own muscle and area of skin. Affected nerves may cause paralysis of one or multiple muscles, numbness or tingling. Since coughing, sneezing or straining causes the pressure in the spinal canal, and therefore the pressure exerted on the sciatic nerve, to increase, the pain radiating down the leg may temporarily become more intense. We can often tell from a patient’s description of his leg ache and of the nature of any loss of strength that may have occurred which nerve has been affected.
Diagnosis of a spinal hernia
Neurological examination and medical imaging
Following the neurological examination, we perform a medical imaging procedure to determine whether the pain in a patient’s leg is indeed caused by a bulging intervertebral disc. Generally, an MRI scan of the spine is the type of medical imaging procedure performed when a doctor suspects a spinal hernia.
At our clinics, MRI scans can either be performed at once or soon after the patient’s intake interview. MRI scans have the advantage of being able to create an image from three directions, and to render the intervertebral disc itself visible, in a manner which tells us more about the extent of its degeneration.

Diagnosis of a spinal hernia
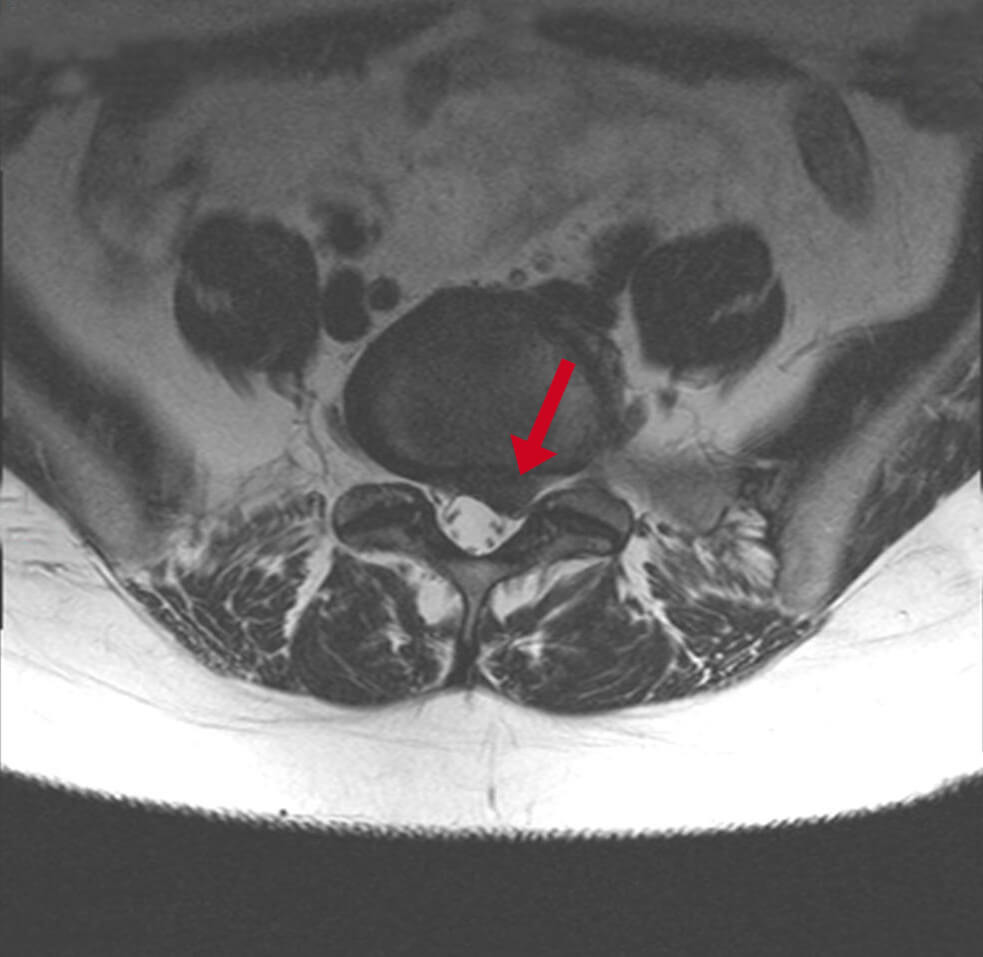
MRI of the spine
Surgery of a spinal hernia
Not every hernia requires surgery
Some 70 to 80% of all hernias heal of their own accord, following rest and physiotherapy. In other words, patients must not rush into surgery. On the other hand, the recovery process may take longer if a patient waits too long before undergoing surgery. Generally speaking, surgeons will wait at least six weeks before operating on a patient (unless there is an indication for emergency surgery), but will want to perform surgery within 6 months of the onset of the pain (if the pain lasts that long).
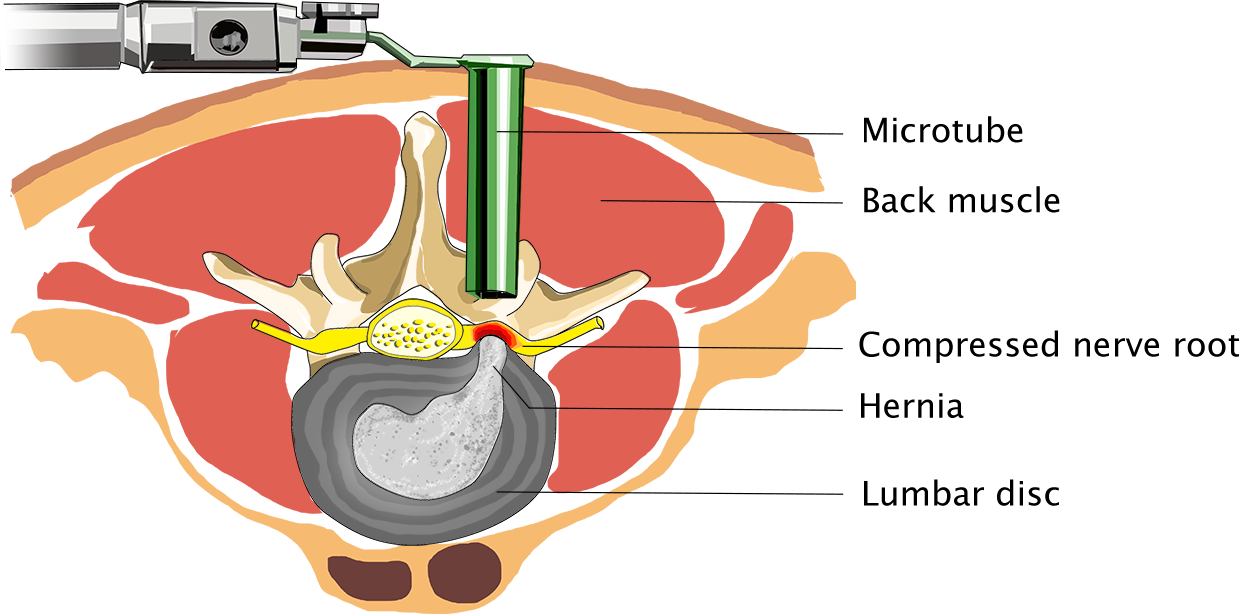
Surgery of a spinal hernia
So what happens when I undergo surgery?
Click the button below for some general information on operations performed by Dr Schröder.
Risks of spinal hernia surgery
Potential post-operative complications
Like any other operation, spinal hernia operations carry a few risks. However, complications are highly unlikely to occur. After all, spinal hernia surgery is performed at our clinics many times a year.
Even so, we may encounter some neurological failure after the operation, which is generally caused by the surgeon’s having had to manipulate a nerve that had been compressed for a long time. Common risks also include inflammation of the wound or a wound that does not heal properly. Subsequent bleeding is a much more rare but problematic complication. The well-known cerebrospinal fluid leak is another, none too severe complication. A fluid leak is a tiny tear in the sac that holds the cerebrospinal fluid. When this happens during surgery, the leak will be sealed at once, and it will not have any lasting consequences. In very rare cases a tear may continue to leak after having been sealed. If this happens, the tear will have to be resealed at a later stage.
After surgery of a spinal hernia
Tips from a physiotherapist
Following the operation, the patient’s follow-up appointments will be with a physiotherapist, who will provide some useful tips to help the patient load his back and make a full recovery while the patient is still at our clinics. Typically, patients are able to walk again the day after their operation. They are free to go home, then, depending on the size of their wound.
Follow-up examination
Two weeks after the operation, we will ring the patient for a phone check-up during which we will discuss his or her current condition. Generally, the patient will be told on this occasion that s/he is allowed to resume normal activities and increase the load on his or her back. If the patient is already experiencing a clear improvement, no further steps will have to be taken at this point.
Resuming exercise and returning to work
Patients will be allowed to undergo supervised physiotherapy upon their discharge from the clinic if they are in a poor physical condition or afraid to resume movement. Embarking on an intensive back and abdominal muscle training programme soon after the operation is not recommended, as the back muscle will not have full pulling force for the first 3 to 6 months following surgery. The duration of the post-operative recovery period varies from patient to patient. Whether or not a patient will be allowed to return to work soon after his or her operation obviously depends on the nature of the person’s duties. Patients should always listen to their bodies and take a break when their bodies tell them they have had enough.






